CLINICAL UTILITY OF BONE MARKERS
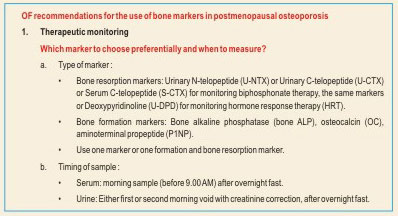
Therapy Monitoring
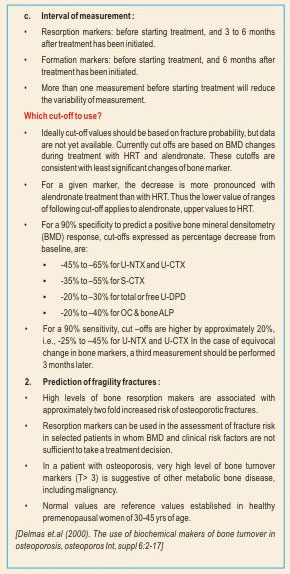
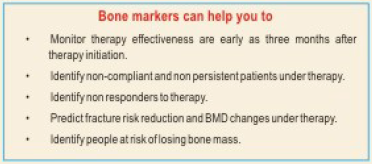
The most persuasive evidence to date for the use of bone markers is in the area of monitoring of osteoporosis treatment. The aim of the treatment is to prevent fractures. Biphosphonates, estrogens and ralozifene decrease bone resorption and bone formation markers.; strontium ravealte treatment causes a mild reduction in bone resorption markers and a slight increase in bone formation markers; teriparatide (recombinant PTH) increases both bone formation and bone resorption markers. The advantage of suing bone markers instead of BMD is the significant changes in the bone markers can be observed after three to six months after initiation of therapy, whereas changes in BMD becomes significant only after 18 to 24 months; a long time to detect treatment failure. The reduction in fracture risk following antiresorptive treatment was seen early similar to change in bone markers, whereas the change in BMD are gradual and later. No surprisingly change in bone markers explains a much greater proportion od reidction in fracture risk than any change in BMD. Taken together, these data suggest bone markers are arguably better tools than BDM for monitoring antiresorptive treatment.
Fractures risk assessment
The diagnosis of osteoporosis is based on bone density scanning by virtue of WHO definition of osteoporosis and patients with a low bone density have increased risk of fracture. However a considerable body of data indicates that bone markers predict bone markers predict bone loss independent of bone density; individuals with increased bone turnover loose bone at a faster rate than subjects with normal or low bone turnover markers. Bone turnover markers, in combination with other risks factors of osteoporosis fractures, may be used to describe fracture risk or intervention thresholds. The relative fracture risk, as defined by either low BMD or an increased bone turnover marker, I similar and increased fracture is accentuated when both are present. Thus, in clinical practice, increased bone turnover markers in the presence of a low BMD would favor initiation of treatment for that patient.
To identify noncompliant patient
Bone markers react very sensitively and quickly (within days) to irregular drug taking and therefore rapidly reveal inconsistent intake of medications. Positive feedback to the patient has been shown to improve the patient’s adherence to the prescribed medication. Studies have shown that up to 50% of patients stop treatment too early and medication is taken irregularly. Adherent patients were shown to suffer fewer fractures and to incur lower hospital costs.
To identify non responders to therapy
Most therapies are highly efficient as proven in many studies and true treatment failures are rare. However there are some patients who do not respond to therapy for the following reasons:
- Malabsorption
- Alcoholism
- Immobilization
- Glucocorticoid treatment
- Hyperthyroidism
Bone markers are able to identify these patents at a very early point in time to allow for appropriate measures to prevent future fractures.